The Long COVID Brain Drain
- Home
- Blog

The negative impact of COVID on the brain’s mitochondria—the tiny "power plants" of cells—can lead to long COVID brain fog, anxiety, and depression. Luckily several strategies, including lifestyle interventions, can help long COVID patients find relief. In this blog, we will cover:
- The connection between long COVID and mitochondria
- Mitochondria’s role in the brain fog pandemic
- How mitochondria can influence long COVID patients
- Treatment options for long COVID symptoms caused by damage to mitochondria
- How Root Cause Psychiatry can help diagnose and treat long COVID
Is Long COVID Brain Caused by a Mitochondria “Energy Crisis”?
My Dear Readers, your brain is responsible for powering up your thoughts, feelings, behavior, creativity, and consciousness—and as you might imagine, all of these tasks require a lot of energy to be successful. Our brains weigh a mere 3% of our body’s mass, yet they must produce and then consume 20-25% of the total energy the body needs to operate. Mitochondria are the extremely tiny “power plants” behind all of this energy production. For their size, each mitochondria creates the energy equivalent of a lightning bolt!
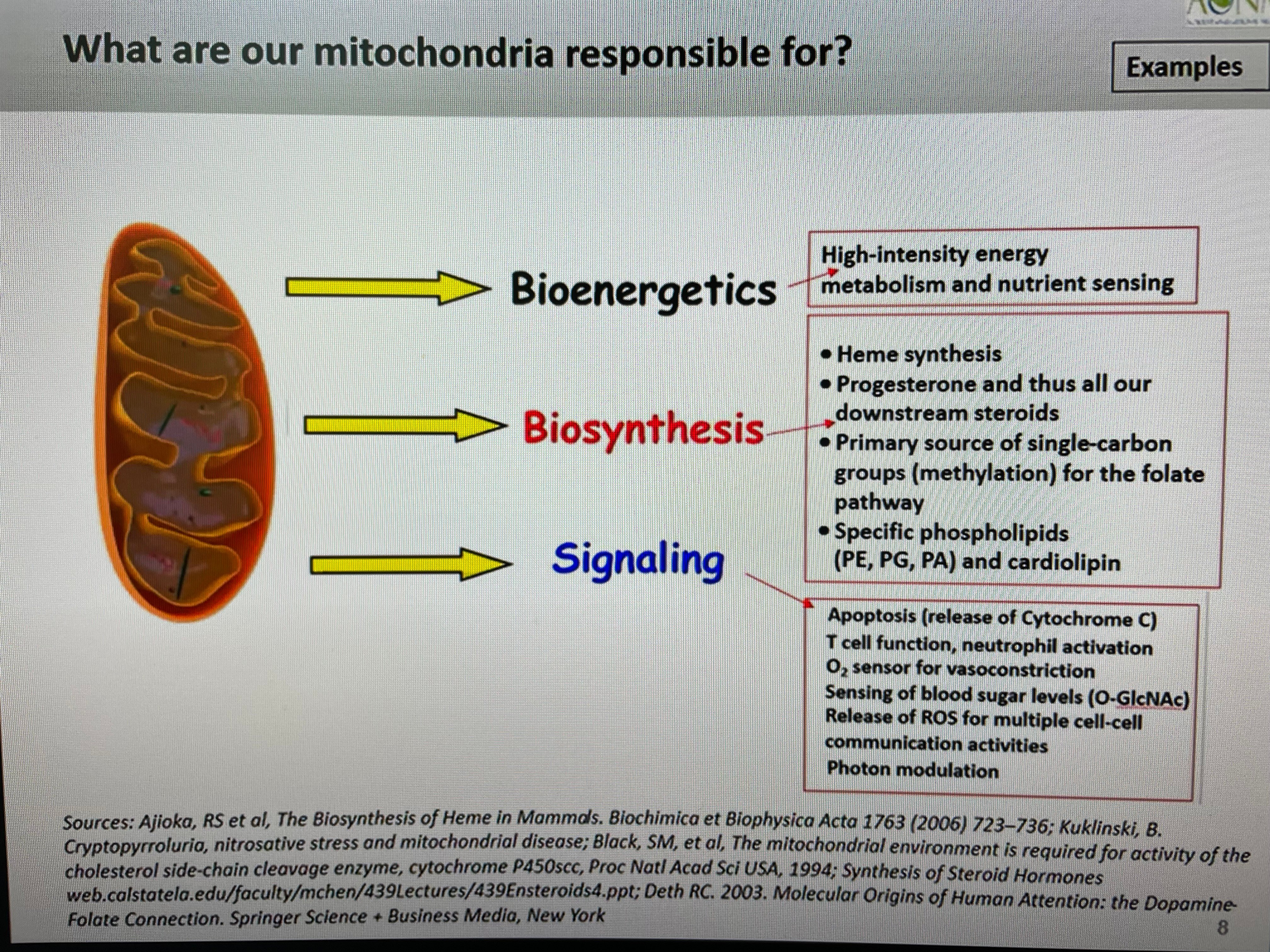
Mitochondria perform thousands of functions a second within each of your brain cells. The infographic below summarizes many of them. But when that functioning is disrupted, your brain gets disrupted too. Emerging science shows that COVID can directly cause the mitochondria in your brain to self-destruct—which in turn can lead to long COVID brain fog, anxiety, and depression. In other words, damaged mitochondria can lead to an “energy crisis” in your brain. Could this be one of the root causes of long COVID—and if so, what can you do about it? Read on to find out.
Mitochondria’s Role in the Brain Fog Pandemic
In prior blogs, I explained long COVID as a “Brain Fog Pandemic” and outlined a number of possible causes, including persistence of the virus or viral fragments, reactivation of other viruses—like Epstein Barr Virus (mono) or Lyme Disease—from prior infections, autoimmunity, tissue damage causing chronic inflammation, and gut dysbiosis. I also outlined the role of micro blood clots in perpetuating the misery of long COVID, and how our immune system can attack our brain cells through “friendly fire” by confusing brain cells with the coronavirus itself.
But another important possible cause of long COVID takes place when healthy mitochondria get hijacked by the COVID virus, leading to their disruption. You see, when the COVID virus infects a cell, it “hijacks” the cell to begin reproducing itself. This process, known as “viral replication”, consumes a tremendous amount of energy to help it manufacture trillions of viral particles. That energy comes from “highjacked mitochondria” which are indirectly appropriated for the virus’s energy supply. Thus, instead of powering up the brain’s important functions mentioned earlier, mitochondria power up the virus’s manufacturing plant—and in the process become damaged.
How Do Mitochondria Influence Long COVID Cases?
When mitochondria get hijacked by COVID, long COVID can take root. Below are just a few ways in which this can happen—and why.
- Scientists believe that, prior to a patient being infected, the mitochondria in many long COVID patients were already compromised—perhaps from chronic inflammation due to gut microbiome problems, obesity, Type 2 Diabetes, or other causes. The virus worsens any pre-existing chronic inflammation, which causes further strain on the mitochondria, which in turn begin to release large quantities of “free radicals” that damage both their own DNA and the DNA of brain cells. We have well over 200 billion brain cells that co-exist and communicate in circuits and systems, and this mitochondrial damage, combined with inflammation attacking those cells, can result in long COVID symptoms such as brain fog, depression, anxiety, PTSD, panic attacks, and even psychosis. The damage can also accelerate the aging process of our cells through “inflammaging.”
- The virus also shifts cells from using mitochondria for a fuel-efficient, high-powered means of producing energy to a less efficient production system outside the mitochondria. Mitochondria are 18 times more effective in producing energy than the other cellular mechanisms, so this shift dramatically reduces energy production needed to power all cellular functions. This results in physical fatigue including exercise intolerance, mental fatigue, and long COVID brain fog.
- The direct damage the virus may create in brain cells also causes those cells to” leak” mitochondria out into the bloodstream, which triggers further brain inflammation. This same leakage also activates blood platelets to produce the micro blood clots I discussed in a prior blog, which narrow blood vessels and starve mitochondria of the oxygen and nutrients they need to function. All these factors contribute to long COVID brain fog, depression and other psychiatric symptoms.
- Research also suggests that a protein on the surface of the SARS-CoV-2 virus can directly cause mitochondria to self-destruct. Think of the coronavirus here as inducing a kind of “mitochondrial suicide,” which further lessens the power supply needed to properly fight off the initial infection and power up necessary cellular repair functions once the virus has been cleared.
- The virus has also been associated with creating problems in the “gut-brain axis”. There are many similarities between the effects of a COVID-19 infection and inflammatory bowel disease, in particular dysbiosis and its associated “leaky gut, leaky brain, leaky emotions”. It is now well recognized that there is two-way communication between the gut microbiome and the brain’s mitochondria, which can influence mitochondrial energy production and how mitochondria regulate the immune system. In turn, mitochondria regulate gut function, inflammation, and gut wall integrity to prevent leaky gut syndrome. COVID’s impact on mitochondria likely disrupts this fragile cycle, leading to gut concerns.
Treating the Energy Crisis in Long COVID Brain Fog and Depression
Now that you know some of the ways in which COVID can disrupt your mitochondria and lead to long COVID brain fog, depression, and more, you are likely wondering: what can I do about it? It turns out, you are far from powerless to power up those damaged mitochondria. Below are a few ways in which you can improve mitochondrial function to take control of your long COVID symptoms. Please speak to your treating physician before implementing any of these interventions.
- A healthy diet and lifestyle may help protect against long COVID brain fog and other symptoms, and is an important aspect of recovery. When mitochondria are in optimal health, they have plenty of reserve energy-generating capacity to both ensure a good immune response and produce powerful antioxidants to resolve inflammation. Healthy mitochondria can also provide sufficient power to immune system cells to destroy the virus more effectively.
- More specifically, a healthy plant-based diet could help treat long COVID symptoms. Plant-rich diets contain lots of phenolic compounds, which are well known to modulate mitochondrial function toward health in a number of ways.
- Another approach is to restrict calories, as this is a well-known way to reverse many metabolic dysfunctions. For instance, a ketogenic diet stimulates mitochondrial function. And calorie restriction stimulates mitochondrial renewal—another possible way to help patients recover from COVID-19.
- Hormesis is the application of a mild, short-lived stressor to our cells, and is generally used to create a healthier, longer lifespan. Hormesis may help patients suffering from long COVID. In some patients this may include light exercise (high intensity interval training is to be avoided).
- Another possible approach is to use the NAD+precursor nicotinamide riboside (NR), which has been investigated for the treatment of SARS-CoV-2. NR activates genes that help improve energy production and create new, healthy mitochondria.
- And finally, there are other emerging new treatments, such as photobiomodulation (PBM), including infrared and near infrared lighting to reduce inflammation and improve mitochondrial functioning.
How to Assess and Treat Mitochondrial Malfunction using Root Cause Psychiatry
Root Cause Psychiatry uses tests such as Genova’s NutrEval and Metabolomix to determine levels of oxidative stress and mitochondrial dysfunction; the Vibrant Gut Zoomer to assist with determining the presence of gut inflammation, dysbiosis, and leaky gut that disrupt the gut-mitochondrial communication pathways; IntellxxDNA to uncover genetic vulnerabilities to mitochondrial dysfunction and ways to “turn on and turn off” harmful genes; and numerous biomarkers of inflammation and blood micro clots which can be assayed through LabCorp, Quest, and IncellDX.
At Potomac Psychiatry we use these tests to help evaluate and treat our patients with long COVID brain fog and depression by accurately pinpointing the root causes of their condition, and providing precise interventions such as antioxidant support, micronutrient supplementation, anticoagulation, anti-inflammatory supplements, and the use of prescription medications when indicated.
If you or a loved one are suffering from long COVID, feel hopeful that a number of interventions are possible to help alleviate your suffering and restore your health.
.png?width=144&height=144&name=Untitled%20design%20(34).png)