Long COVID Spike Proteins Cause a Mighty Moody Microbiome
- Home
- Blog

- Long Covid Spike Proteins
- Microbiome Significance
- The Gut Microbiome and Acute COVID Infection
- The Relationship Between Acute COVID, Long COVID and the Gastrointestinal Tract
- Spike Proteins Persist in the Gut, Possibly Causing Long COVID Brain Fog and Depression
- Gut Healing to Treat Long COVID Brain Fog and Depression
Long Covid Spike Proteins Cause a Mighty Moody Microbiome
My dear reader, I hope this blog post finds you well, with life finally returning to normal following COVID. Sadly, life has still not returned to normal if you are one of the millions of people suffering from long COVID symptoms, such as brain fog, depression, anxiety, or obsessive-compulsive disorder (OCD), and undoubtedly, what you want more than anything is to just get your old life back.
Let me try to help you achieve that. This fifth blog post in my long COVID series was written to help you learn more about how your gut microbiome may cause or contribute to it and what can aid in recovery.
The Microbiome’s Significance
The microbiome is so important to our mental health. I have written well over 50 blogs that feature it!
Previous long COVID blogs have covered numerous other causes. These include but aren’t limited to micro clots in tiny blood vessels, antibodies that attack brain cells, and damage to mitochondria (those “power plants” and major manufacturing centers inside our cells). Today we will focus on those 100 trillion “bugs” that live in your large intestine and can exert a huge influence on perpetuating long COVID.
Prior blogs on the gut microbiome cover its role in worsening many other conditions, such as depression, autism, Alzheimer’s disease, bipolar disorder, OCD, ADHD, and more. Take these astonishing examples: A fecal transplant from children with autism into normal mice causes “autistic mice,” and a fecal transplant of normal microbes into mice bred to develop “mouse dementia” improved their cognitive functioning and reduced amyloid protein deposits in their brains—the same proteins that build up in the brains of human Alzheimer’s patients!
The Gut Microbiome and Acute COVID Infection
The gut microbiome is a complex ecosystem of 100 trillion microorganisms that live inside our digestive tracts. These “bugs” include bacteria, viruses, and fungi that play a crucial role in the overall well-being of our bodies and minds. In other words, they help us perform the following necessary biological functions:
- Digest food.
- Absorb nutrients.
- Program and regulate the immune system.
- Produce neurotransmitters, hormones, and vitamins.
- Protect against harmful diseases and toxins.
Studies have shown that COVID-19 can affect the gut microbiome in several ways. For example, a study published in the World Journal of Gastroenterology found that patients with COVID-19 had an altered gut microbiome compared to healthy individuals and had lower levels of beneficial bacteria (Bifidobacterium and Lactobacillus) and higher levels of harmful bacteria (Veillonella and Actinomyces).
Another study published in the journal Gut found that COVID-19 patients who had gastrointestinal (GI) symptoms, such as diarrhea, nausea, and vomiting, had a more significant disruption of their gut microbiome than those who did not have GI symptoms. Results suggested that the virus had depleted their gut of beneficial bacteria, which led to an overgrowth of harmful bacteria.
The Relationship Between Acute COVID, Long COVID and the Gastrointestinal Tract
Some studies have addressed that the numerous acutely ill COVID-19 patients with GI symptoms may be at higher risk for developing long COVID.
The mechanisms by which COVID-19 affects the gut microbiome are not yet fully understood. However, some researchers believe that the virus may enter the GI tract through the mouth and infect the cells lining the digestive tract, leading to inflammation and damage to the gut microbiome. Other researchers suggest that the virus may indirectly affect the gut microbiome through the immune system's response to the infection; 70 percent of our immune system resides in the gut.
Many believe that these changes contribute to the development of long COVID. For example, one study found that the gut microbiome of long COVID patients (not just the acutely ill group of patients described earlier) was depleted of beneficial bacteria (Bifidobacterium and Lactobacillus) and had an overgrowth of harmful bacteria (Clostridium and Streptococcus). Findings suggest the initial depletion of good bacteria may persist for a long time.
Another study found that patients with COVID-19 who experienced GI symptoms as a part of their acute illness were more likely to have persistent symptoms several months after their acute illness had resolved. They were also more likely to experience ongoing symptoms, such as fatigue and difficulty concentrating (“brain fog”) during follow-up.
Another study found that COVID-19 patients with GI symptoms during their acute illness had a higher risk of developing long COVID. They were also more likely to experience persistent symptoms, such as fatigue, joint pain, and difficulty sleeping, six months after their initial diagnosis.
Spike Proteins Persist in the Gut, Possibly Causing Long COVID Brain Fog and Depression
Another study found that COVID-19 patients with GI symptoms during their acute illness had a higher risk of developing long COVID. They were also more likely to experience persistent symptoms, such as fatigue, joint pain, and difficulty sleeping, six months after their initial diagnosis.
Persisting spike proteins from the coronavirus that remain in the gut for long periods of time may contribute to the development of aforementioned long COVID symptoms, including fatigue, depression, and brain fog.
A study published in the journal Nature found evidence of SARS-CoV-2 spike proteins in the gut lining of people with long COVID and not healthy control subjects. They suggest that this presence could contribute to ongoing inflammation and other symptoms.
Another study published in the journal Lancet Respiratory Medicine also found evidence of SARS-CoV-2 RNA in the gut microbiome of people with long COVID. The researchers analyzed fecal samples from patients with long COVID and healthy controls and found that the viral RNA was present in significantly higher levels in the long COVID group. They suggest that this could contribute to ongoing immune activation and inflammation.
Two small studies associate these types of findings with persisting brain fog. One study found that individuals with long COVID had altered gut microbiome composition compared to healthy individuals and that these changes were associated with symptom severity, including brain fog.
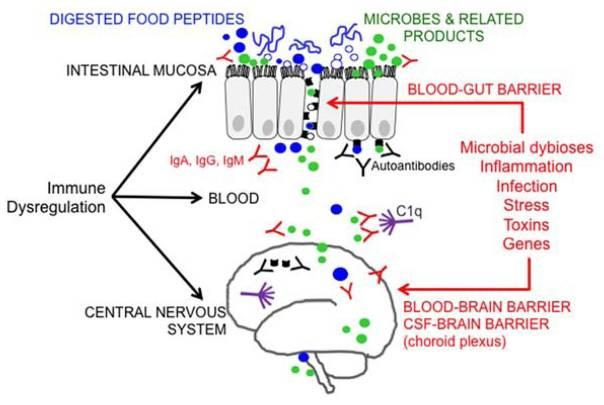
And finally, a recent study published in Frontiers in Cellular and Infection Microbiology ties all of this together. It discusses how the gut microbiome undergoes significant alterations in response to SARS-CoV-2 and suggests that the long-term neuropsychiatric symptoms of COVID-19 may be related to these alterations. For example, neuropsychiatric conditions such as Guillain-Barre syndrome, chronic fatigue, psychiatric disorders such as depression and anxiety, and even neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease may result from how COVID alters the gut microbiome. How? One cause may be the inflammatory cytokines that are released that “set your brain on fire.”
Another COVID cause may be gut inflammation resulting in dysbiosis and leaky gut syndrome in part due to shortages in the production of short-chain fatty acids (SCFAs), due to a decrease in the number of beneficial bacteria that are known to produce SCFAs (e.g., Faecalibacterium prausnitzii).
In a prior blog post, I discussed how lower numbers of these bacteria are also associated with bipolar disorder. These causes are illustrated in the gut-brain axis infographic below.
Gut Healing to Treat Long COVID Brain Fog and Depression
If you or a family member is suffering from long COVID, feel hopeful that you can begin to heal your gut microbiome starting today! There are several potential ways to support the health of the gut microbiome during and after a COVID-19 infection. For example,
- A healthy diet rich in fiber and fermented foods, such as yogurt and kefir, can promote the growth of beneficial bacteria in the gut.
- Probiotic supplements may also be helpful in restoring the gut microbiome after a COVID-19 infection.
- Lifestyle changes such as stress management, sleep, and exercise can also support the health of the gut microbiome. Chronic stress has been shown to negatively impact the gut microbiome.
- Wellness strategies such as meditation and yoga may be helpful to reduce stress and restore healthy microbes while eliminating unhealthy ones.
Learn more about our long COVID depression and brain fog treatment program. If you are suffering from long COVID and would like a no-cost 15-minute consultation with Julie Wendt and me to describe how we evaluate and treat patients suffering from this condition, please call 301-984-9791 and ask for Dana Schwartz, or email Dana at info@potomacpsychiatry.com.
.png?width=144&height=144&name=Untitled%20design%20(34).png)