COVID “Wear and Tear” – Six Genes – Sixteen Solutions
- Home
- Blog

Biohacking Your Mental Health Ecosystem: Part Six
“It is not stress that kills us. It is our reaction to it”
― Hans Selye, MD, PhD, “The Stress of Life”
Reader, here’s a pop quiz: What day is it today? If you aced that question, how about this one: What month are we in? Now for a more reflective question: What day or month does it feel like? In these pandemic times, where our homes have become both our sanctuaries and our prison cells, those first two questions can feel almost laughably hard to answer. What’s the difference between a Tuesday and a Friday when all our days are consumed by the same 14 inch monitor? What’s the significance of a balmy summer weekend when we are without any occasion whatsoever to wear our fun hot-weather clothing? That last question I posed is stranger still: the quarantine and its after-effects brought a great pause into our lives in March… yet many of us are still waiting for someone to press “play” once again. To the folks I speak to, there’s a strange sense that time has somehow ceased to move forward. With our social calendars on hiatus, our doctor’s appointments postponed, and our plans for the future put on an indefinite hold, much of our daily lives certainly prove that sense out. All the more alienating, then, to see our bodies gradually grow bigger or softer from stress eating or lack of exercise—to see our hair still in need of a cut, our children maturing before our eyes… and so on! Never before in my memory has there been such a collective unease about the inevitable passing of time. In the blink of an eye, in the midst of that global pause, many of us have awoken to lives that have changed dramatically—and many of us have no account of how those changes happened. This is especially true when it comes to our mental health. I have seen many patients these last few months who are baffled by their sudden onset of anxiety or depression—and sadly, the confusing nature of it all only makes them feel worse. Time is indeed moving forward, and while that can mean mental health symptoms can worsen in this global crisis, it also means they have the potential to improve, too. Just because we may feel a pause on our lives and dreams does not mean we cannot begin a journey towards healing, whatever that may look like. In this blog, I am excited to share with you some scientific background as to why this time feels so heavy to all of us, why your genetic code may be exacerbating these already difficult times, and how I helped one of my patients re-frame this crisis as an opportunity to seize the reins of her own life, using the results of her genetic tests to feel better than ever. If you or a loved one is experiencing anxiety or depression, I believe you will relate to her tale. Let’s dig in!
Allostatic Load and Overload: A Chronic, Caustic, Coronavirus Bully and Human Evolution
Over the eons, as millions of life forms have emerged here on earth, important systems have evolved inside them to “buffer” the shifting environmental effects on their living cells. To survive, all living organisms must maintain what is known as homeostasis. Environmental stressors constantly threaten to disrupt homeostasis in our cells. When we lived in the wild, the main threats to our health and well-being were acute stressors, such as predators, injuries, infections, starvation, and changing weather. These life-or-death threats could materialize at a moment’s notice, so biologic systems developed to protect and maintain our homeostasis, known as “allostatic systems,” that could modulate our response to stress.
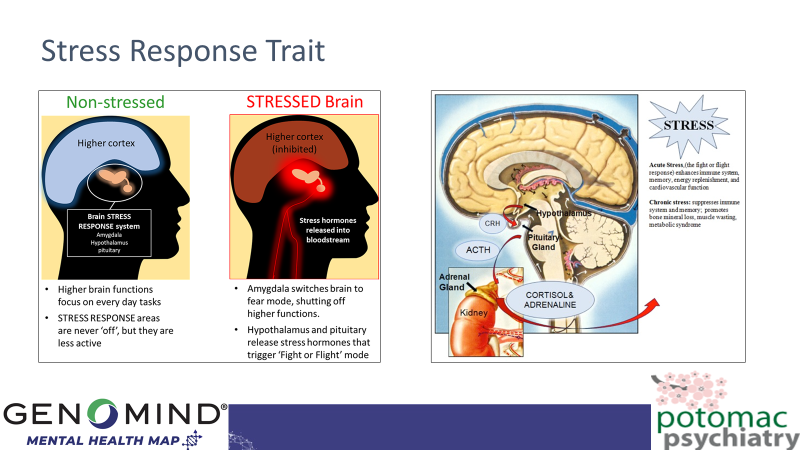
One such system is our “Fight or Flight” response. Mediated by hormones from our adrenal glands (cortisol and adrenaline), this system rapidly enables us to fight off threats by boosting our heart rate, mitochondrial energy production, immunity, and muscle strength.
In the modern world, these sudden stressors have been largely replaced by chronic stressors which produce “wear and tear” and “overload” of the stress response systems. This results in inflammaging of our cells, and many chronic diseases including obesity, type 2 diabetes, atherosclerosis, autoimmunity, allergy, and certain psychiatric disorders.
We can now add Coronavirus-SARS2 to the list of chronic stressors that plague our emotional health. We are now six months into the global pandemic with no end in sight. The chronic emotional effects of this massive, invisible global bully might be described as “wear and tear” on our emotional life, which may include a weakening of our immune system response, known as “allostatic overload”. Rather than wring our hands and feel helpless and hopeless, what can we do to fight the stress caused by this ultimate bully?
As this blog will describe, our underlying genetics can determine how we and our loved ones and employees can build both emotional and immune system resilience to defeat that coronavirus bully. You see, certain genetic variations in SLC6A4, COMT, BDNF, and OXTR genes predispose us to “allostatic overload” and yet we now have proven epigenetic interventions to address each of these genetic vulnerabilities. As a gentle reminder, the gene-based treatments I present below are not recommendations for you to follow. Please do not implement any of these treatments on your own—you should always consult with a licensed mental health professional first.
Am I an SLC6A4, COMT, BDNF, or OXTR Orchid?
“Every genetic ‘illness’ is a mismatch between an organism’s genome and its environment. In some cases the appropriate medical intervention to mitigate a disease might be to alter the environment.”
― Siddhartha Mukherjee, M.D.

Those who possess a SLC6A4 S/S or L(G)/S orchid gene suffer from an overactivation of the amygdala—the emotional center of the brain—when chronically stressed. This genetic variation is often best treated by a change in environment to a less stressful environment. With respect to prescription medications, SNRIs and Trintellix may also be helpful in treating symptoms of anxiety and depression.
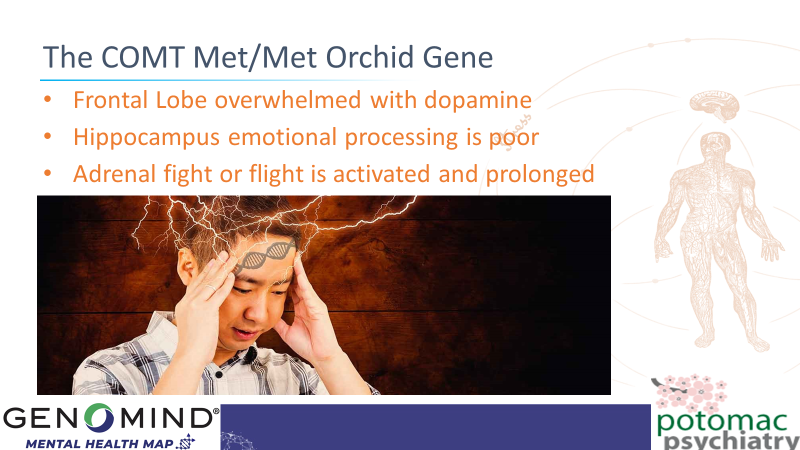
Those who possess a COMT Met/Met orchid gene suffer from flooding of the brain’s frontal lobes with dopamine when placed under chronic stress, and are less able to process strong emotions as frontal lobe and hippocampal functions are overwhelmed. Potential treatments include n-acetylcysteine (NAC), ashwagandha, magnesium, and second generation antipsychotics.
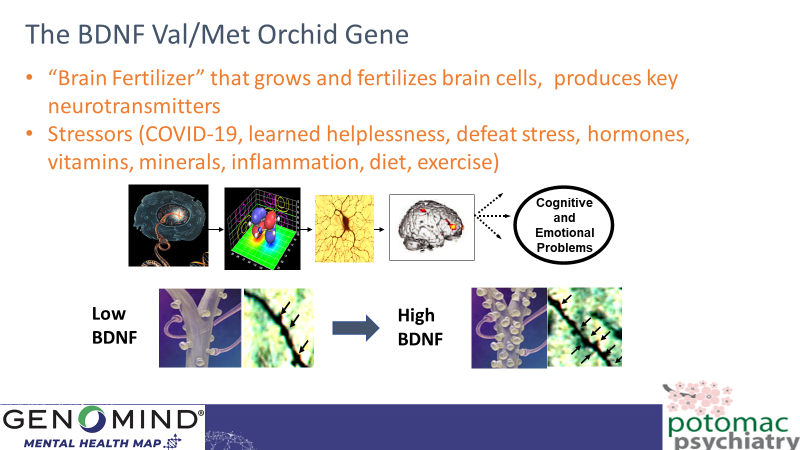
Those who possess a BDNF Val/Met or Met/Met orchid gene suffer from a “withering of the brain” in response to chronic stress, as protein levels of BDNF, “the brain’s fertilizer” drop. The brain cells and their synaptic connections are less protected from the inflammation and oxidative stress resulting from “wear and tear”, and thus the brain’s circuits and systems that help with emotional regulation, cognition, and working memory begin to malfunction. Possible treatments include exercise, high dose omega 3, and lithium.
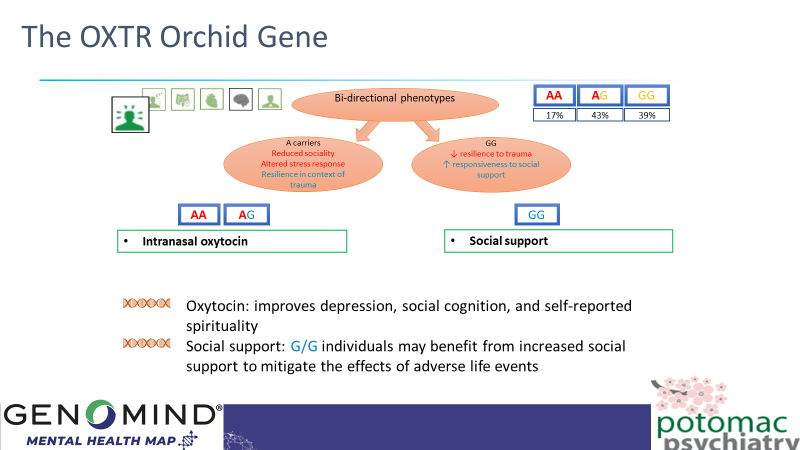
Oxytocin is the brain’s “comfort food” hormone. It is also known as the “bliss hormone” as it is found in higher levels in the bloodstream of mothers, fathers, and infants who are actively bonding. In response to chronic stress it would help boost your emotional resilience to have higher levels of oxytocin inside your brain, and, depending upon your genetic variation of OXTR, that might involve increasing your social connections with others or intranasal oxytocin which will directly enter your brain.
Pandemic Anxiety: FKBP5 and CRHR1—Adapting through “Adaptogens”
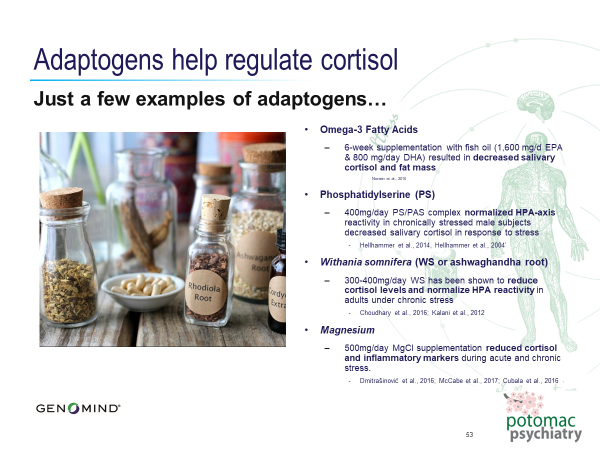
If you have a T allele on your FKBP5 gene, you may be predisposed to higher levels of stress. This variant confers a dysregulated cortisol response to stress, fails to “turn off” your stress response, decreases your ability to “come down” after a stress response, and has even been shown to possibly increase the risk of depression following trauma. If you have a G allele on your CRHR1 gene, you may be prone to significantly increased levels of cortisol in response to stress, as well as poor working memory and increased rates of depression. In other words, if you have one or both of these variants, you very likely have an atypical and heightened response to stress. Lifestyle changes and supplements can help you regulate and decrease your response to pandemic-related stress over time. These include meditation, exercise, St. John’s Wort, Phosphatidyl Serine, N-Acetylcysteine (NAC), Vitamin D, neurofeedback with QEEG, Ashwagandha, and Agmatine.
The story of Jennifer, an “Amygdala Orchid” with “Fight, Flight or Freeze Genes” too
Jennifer returned to see me after a ten year hiatus. She had done really well in our work together years ago, and while I was happy to see her again, I felt concerned about why she felt the need to come back. “Doc, I’m in bad shape right now—so bad that I have taken a medical leave of absence from work. I have been feeling anxious and depressed, have put on a lot of weight, and am worried about losing my job, particularly since I am taking time off. On the other hand, the time off has been wonderful, as I have had more time to be around my wife and the kids for the first time in years. I realize how much work has consumed me, and how much I have missed them as a result.” She then began to cry uncontrollably. “Jennifer, I am sorry you are feeling so sad and scared, and am glad you returned to seek help. Let’s run through some rating scales to determine the type and extent of your symptoms of anxiety and depression, and then I want to talk with you about two new genetic tests we have implemented to better understand your underlying genetic vulnerabilities and how to address them.” She scored in the moderate to severe range on the Beck Anxiety Inventory and the Beck Depression Inventory, and had suicidal thoughts, but no plans or preparations to harm herself. “Jennifer, please update me on your career since we last spoke ten years ago, as I recall you were working in venture capital at that time, do I remember correctly?” “Yeah Doc, at that time I was in venture capital, and about five years ago moved over to private equity at Warburg Pincus in New York City. It meant I had to commute there and spend three days a week away from home which has been hard, given that my kids are growing up largely without my presence in the home. But I couldn’t pass up the offer as the compensation is such that my wife and I will be ‘set for life’ in another ten years if I stick it out. Now I’m not sure I want to given how much I realize that I’ve missed my family so much. And then this COVID thing hit, and our portfolios took a big nosedive, and my superiors responded with tremendously increasing the pressure on us, at times even yelling and screaming at me. Eventually I couldn’t take it anymore, couldn’t focus or concentrate on my work and began crying every day, and so I had my primary care doctor fill in forms to grant me a medical leave.” As I listened to her update, it was apparent, even over Zoom, that she was just so sad and scared, and so stressed-out, and yet was clearly loving the time with her family. “Jennifer, I am confident that we can work together to figure out both how to help you fully recover from your anxiety and depression, and how to help you with those life-stage issues around missing your family, career goals, and personal and professional growth. First, let’s focus on understanding what is going on with you biologically, and to that end I will order some blood tests and tell you about those two genetic tests—one is prescription medication oriented, and the other is oriented toward supplement, nutrition, and lifestyle management. Which would you prefer?” Jennifer thought for a moment and said, “I’ve never been a halfway-in person, Doc, so I want both tests!”
And so we direct-shipped to her home the Genomind Professional PGx and Genomind Mental Health Map tests, and with two simple cheek swabs she sent them away for analysis. When the results came back a week later, it was interesting to note that she had a number of genetic variations that helped explain what happened to her: On Professional PGx we determined her personal genome included the SLC6A4 S/S “orchid gene,” the CACNA1C A/A gene, and other variants related to how some medications would be metabolized slowly in her body, while others would be metabolized very rapidly, thus affecting how we would dose prescription medications; and variants in her CRHR1 and FKBP5 genes, which could be addressed with supplements. I explained to her, “Jennifer, you have a number of vulnerability genes here that we will address systematically. I recommend that we start you on Trintellix which will work well to help your symptoms of depression and anxiety, given your SLC6A4 and drug metabolism genes. For your CACNA1C variant, which means the neurons in your brain are over-excitable which is associated with the mood swings, irritability, and temper outbursts you’ve been having, I recommend we start high dose omega 3, and speak with your internist about switching your amlodipine to nimodipine (both are blood pressure drugs, but the latter crosses the blood-brain barrier to better regulate that CACNA1C gene). In addition we will start you on NAC (n-acetylcysteine) and Ashwagandah to modulate the negative effects of those stress genes, CRHR1 and FKBP5. I also recommend you read the book, Dancing with Life by Phillip Moffitt to help you learn how meditation can help reduce your response to stress. What do you think of this initial plan?” Jennifer nodded agreement (over Zoom, of course) and then asked me, “What about my work? The leave of absence? Do you have any thoughts?” And in response, over the next few sessions we developed a short term, intermediate term, and long-term plan for this highly talented and driven “orchid.” In the near term she would remain on a leave of absence until the medication and supplement regimen began to alleviate her symptoms, and intermediate term she would work from DC and no longer commute to New York, and would negotiate this with her employer. And in the longer term…? We began to explore her becoming a University Professor, a lifelong dream that might just be time to evaluate more closely!
The Pandemic and our Human Ecosystem
Reader, stay-at-home orders, the face masks, and social distancing efforts save lives—and they must be implemented at all costs. But it would be foolish for us to disregard just how significant a role these factors play in our growing feelings of isolation. Many of my patients have not seen their family or friends in months—and for many, an online presence makes a poor substitute at best—and a toxic one at worst. And yet, somehow, this time of isolation has only served to underscore our shared humanity, and the universality of our human thoughts and emotions. We are all struggling right now—and if we can lean into our shared hardships a little further, we can see just how interconnected we really are. A global dis-ease is upon us—but just as time keeps moving forward, bringing with it the possibility of hope, so, too does this moment offer a chance for us to dream of a better future: one of global ease, a breath of relief. One by one, and then together, we can bring this future to life.
For Employers and HR Professionals
If you are an employer or HR professional, undoubtedly one of your major sources of chronic stress relates to assisting your workforce to cope with chronic COVID stress. Perhaps this global webinar featuring international HR and psychiatric leaders, could be of help.
Related Information
- Learn about Genetic Testing
- Learn about Potomac Psychiatry
- Meet Our Doctors
- Contact Potomac Psychiatry
.png?width=144&height=144&name=Untitled%20design%20(34).png)



